|
I am a carrom board. Just a piece of wood. Happy to help. They enjoy playing on me, whenever they can, wherever they can—in the corridor, on the lawn or in a room. When they are all around me, playing or encouraging the players, you can’t tell the patients from the family. Of course, if you were around the day I was on the tray table and you found them applauding every feeble strike that just managed to touch a coin, you would have known that they were trying to cheer up the once-brilliant high-school teacher on the bed, who was depressed because now she could not even manage to teach her 10-year old son. Otherwise, who is patient, whose patient, who is family, whose family—these are all irrelevant questions. One of my players once described me more philosophically. We are all helpless coins, she said. Every pocket is a state of mind: joy, anger, sorrow, and acceptance. The striker is not in your control, and no one knows where you will land next. I don’t understand all that. I am a piece of wood, just a game that may help you forget tomorrow and live today. I am just happy to help. Originally written some years ago for the Cipla Palliative Care and Training Centre, Pune.
0 Comments
Does your cure end with your surgery, dressing your wound or restarting your heart? Or is that just the beginning of your recovery? Guess what, they don’t teach recovery and convalescence in medical school. “Many of my tutors seemed to assume that once a crisis of illness has passed, the body and mind find ways to heal themselves,” Dr Gavin Francis, the author of Recovery: The Lost Art of Convalescence recently wrote in The Guardian. “But nearly 20 years as a GP has shown me time and again that the reverse is true: guidance and encouragement through the process of recovery can be indispensable.” Dr Mazda Turel, a neurosurgeon, agrees. “We are not taught this in medical school,” he says. “But if you are attuned enough as a student while you sit in the clinic or OPD with your mentor you can learn it from your teachers in the way they respond to a patient’s needs in the recovery phase, from their ability to patiently answer umpteen questions (most of them repetitive). Eventually you imbibe care and concern, and that’s enough.” Dr E K Ramanandan, a senior ayurveda physician too thinks most doctors pick up on their own how to help a patient through recovery. Dr Nagesh Simha, Medical Director at Karunashraya, considers helping the patient and family through recovery a matter of compassion. “Yes, the doctor’s personal values matter. However, I believe compassion is something that can and ought to be taught.” Recovery matters in an infected worldAs new strains of coronavirus continue to give us all a physical and emotional pounding, the concepts of recovery and convalescence require deeper contemplation. Convalescence is anything but passive. It’s an action that needs us “to be present, to engage, to give of ourselves.” Anyone who has been through the viral infection is aware of the fatigue that follows. Physiotherapists encourage those in post-viral recovery to push the limits of physical effort. Else, “sufferers can become trapped in a cycle of effort followed by collapse,” with each collapse requiring lesser effort. Recovery must act in concert with natural processes. Florence Nightingale believed that “nature alone cures.” She said what nursing had to do was to “put the patient in the best condition for nature to act upon him.” Nature's healing touch apart, people recover more quickly if they think their physician is sympathetic and there for them. Dr Simha remembers the time he was recovering after a major surgery. “There I was, flat on the bed and everyone would be looking down upon me. Except for one doctor who always made it a point to sit so that he could have a conversation at my level. That made a big difference.” “Every illness is unique,” Dr Francis points out. It follows every recovery is unique too. There is no easy solution or a formula. “It’s a landscape we all have to visit sooner or later. From time to time, we all need to learn the art of convalescence.” Thou shall not abandonAETCOM, a manual on attitude, ethics and communication published by the Medical Council of India for the Indian medical graduate, cites a case study. It is a letter to the oncologist from the husband of a patient who succumbed to breast cancer. Here is the gist. “As you may recall, Alka was diagnosed with breast cancer 5 years ago. We rushed to you knowing your reputation as a talented oncologist and we were not disappointed. Your aggressive approach to the disease made all the difference. Alka beat the disease and she lived disease-free for 2 years. We were very happy and still are very grateful to you. “Then the disease came back with a vengeance. Even at this time you did not give up hope and took on the disease like a warrior but then there came a time that it was clear that the disease had won. We were devastated. “Alka looked up to you as a doctor to provide her with support, but it looked like that you were unable to confront the failure. While you did prescribe pain medications and your office helped us find a home nurse, you were reluctant to meet Alka or talk to her. When we called for appointments, your office would tell us to contact our family doctor for pain medications. “When we did get to see you, you would not even look at Alka’s eyes. You would distractedly talk to her, refill her pain medications and dismiss us quickly. It was as if we were seeing a different doctor than the one we had seen when all was well. And when Alka was admitted to the hospital where she breathed her last you would not even come and see her. “We made so many requests for you to come and visit with her. I even called and told you that it would mean so much for her to see you before she departs but you did not. Would it have been too much for you to come and hold her hand for a minute or say a kind word? “We come to you not with the expectation that a cure is always possible but always with the expectation that you will support us in coping with the disease and the tremendous effects it has on our lives. We don't always expect you to succeed but we always expect you to show us care and compassion. You abandoned Alka and us at the time we needed you most. You, sir, abandoned us when we were most vulnerable.” If we reach it before we are ready, our destination can unsettle us. All of us alive have the same destination—death. When we realise it creeping upon us, many of us are not ready to disembark. That is when we need the ashraya (shelter) of karuna (compassion) to help us cope and to let go in peace. Karunashraya, the palliative care centre in Bengaluru has just published Crossing Over, a collection of 35 stories of people whose journeys so ended. It is about how the proximity of that ending affected those who had to leave, those they left behind and the compassionate team at Karunashraya.
When it comes to palliative care, there are courses and experts but no easy answers. There is no room for judgment, but frustration thrives. A gentle touch or a patient ear often helps to ease the pain as effectively as an opioid. Life matters until it is. The idea is to ensure comfort and facilitate closure. Every palliative care professional tries to practice detached attachment. Yet, it is never easy. There is no shutter you can pull down at the end of the day. They must share the tears and fears of one patient after another, day after day. This book is as much a tribute to them as they are about those they care for. As Atul Gawande, the famous writer and surgeon put it, “In the end, people don’t view their life as merely the average of all its moments. Life is meaningful because it is a story. And in stories, endings matter.” Read this book. Because we are all living our stories. You will find no morals in the pages of Crossing Over. You will find acceptance. And gratitude for those who make the ending matter. Four-year old Gulab was at a busy railway station with her father when someone came close and stabbed him. As he lay dying, and as the world around them rushed about its business, she quietly shut the world out. All I knew was Gul was a puzzle and one of the problem cases when I took charge of her and a bunch of other children at the orphanage, where I used to work. Her face would always be blank. No expression at all. Normally, we would quickly know every new child’s likes and dislikes. Gul had been around for weeks. There was no sound, ever. We had to anticipate everything—from washroom breaks to food to even a few sips of water. Once the background story sunk in by and by, I knew that more than psychology, Gul needed to reconnect to love, to belong to someone. Long before he was killed, her father had been the only one for her. Her mother and a sibling had gone away after some family dispute. Being there for GulI started giving her extra affection. I would be with her every possible moment of the day. She would go to sleep on my lap. Whether she responded or not, I would keep up a chatter with her. I would laugh and not bother about her response. I could sense her eyes following me. There was no expression on her face, but her eyes would be on me and would tell me a lot—sorrow, helplessness, loneliness, frustration, depression and so on. Later, she was comfortable enough to put her hands around my neck. Those hands would transmit her unspoken words, her fear, her worries and, simply, her need of a hug and lots of love. She used to wait for me, and her eyes would follow my every act until I finished with the other children. Then I would take her in my lap, hold her hands or kiss her. Others in the orphanage were getting sceptical. I ensured that I did not neglect any other child in my care. Just that the physical and emotional attachment was strongest with her. Though there was no reciprocation of any kind. Depending on the weather and the time of the day, I would often take the children to the terrace. There we had books and drawing materials. I would read them stories. We would draw stuff and sing songs. When playtime was over, all other children would rush down on their own. Gul would stick around until I took her down. That day, the children had run down. I was putting the books away. Gul was there too, as usual waiting for me. Suddenly, I heard a little voice behind me: “paani …” I dropped the book and turned around. Gul was looking at me. She repeated, “paani…”. I grabbed her and kissed her wet eyes. I was laughing and crying. I crushed her to me and just didn’t know what to do or say. Sometime later I carried her down and excitedly shared the news with my colleagues. Gul had spoken. She had asked for water. They had difficulty believing me. Because Gul had clammed up again. Opening up to loveGul started changing. It was slow. She would continue to cling to me. It was quite a task to get her to accept the other “mothers” in the orphanage. Gradually, Gul was as normal as she could be. The day she was taken away by her adoptive parents, I was not sure if I was happy or sad. I was not around to wave bye to her. Maybe it was better that way. Months later, someone told me that Gul was paying us a visit with her parents. I was thrilled. This time I was determined to see her and talk to her, even if she did not remember me. I was in one of the inside rooms and saw them get out of the taxi. Gul was looking taller and prettier. Suddenly, I noticed a change in Gul’s expression. She was looking at the building and it was as if a cloud had passed over her face. I was all set to rush out when I stopped myself. Did the place remind Gul of the dark days of her life? If she were to see me now, won’t it be worse for her? I remained hidden and moved to another part of the building. Far away, I could hear the supervisor calling out for me. I ignored that and moved towards the terrace. Maybe an hour later, I could hear them getting ready to go back. I peeped out carefully. Gul appeared to be happy. Yet, I sensed she did not want to look back and was in a rush to get into the taxi. I waved out more for myself than for her. Once again, I was crying and laughing. Then I gathered myself and went down. There were other flowers needing help to bloom. Based on a true story narrated by Vaijayanti Thakar. Some details have been changed to protect privacy. Art by Shravani Panse.
Dr Sanghamitra Bora State Lead - Palliative Care, Assam Cancer Care Foundation, Guwahati I was chosen to contribute to the Covid-19 mission and asked to supervise infection control in the screening area, potentially the most infectious area. My job started immediately after the nationwide lockdown, on March 22, 2020. When we started, we did not have adequate number of personal protective equipment (PPE). The team started working with whatever was provided. Getting to know a patientOn April 1, I noticed that one of the persons who had come for screening had red eyes. As he waited in the queue, his body language appeared to convey that he was sick. His wife was in tears. As a palliative care physician, I considered it my duty to talk to her, comfort her and find out what was going on. So, I went to her. Of course, I was maintaining a safe distance. I had put on one N-95 and two triple-layered surgical masks. I was wearing my apron, a disposable surgical gown and three layers of gloves. The wife told me that her husband had a history of asthma going back 12 years. He was on and off medications. Recently he had had fever and an attack of asthma. Their family physician had prescribed some medications. As those didn’t work, the doctor had advised a CT scan of the Chest. The scan revealed pneumonitis, which had prompted their doctor to send him for Covid screening. On probing further, I also came to know that he had travelled to Delhi and returned around February 29, 2020. Meanwhile, her husband was called in by the doctor. That being a screening area, the doctor was supposed to ask questions from a distance of at least two metres. The doctor had two layers of masks and the patient also had to have a mask. To me, it was the perfect situation for a possible miscommunication. Maybe the patient would say “I have fever” and by the time it reached the doctor, he would possibly hear it as “I don’t have fever.” It was important that the doctor filled up the registration form correctly. Because the doctor decided if there was a need to take samples, based on the history as he understood and recorded. The next stop for the form (and the patient) was the laboratory technician who would take samples (if the doctor called for it). I was trying to do what I could to reduce the communication gap so that the doctor was able to record the history correctly. I was trying to talk to everyone who was there for screening to try and avoid any miscommunication. As a protocol I had to recheck the filled-up standard form of sample collection, and hence a second conversation was necessary. I definitely did not want any miscommunication with this particular patient I was observing. Both husband and wife told me they felt really good after they spoke to me. They were advised medications and home quarantine. I told them that if the tests yielded a positive result, the superintendent’s office would contact them. They would be instructed about the standard procedure to follow thereafter. They appeared happy that they had the complete picture. The couple thanked me and went home. Negative times follow a positive result Two days later, I came to know that the man was Covid-positive. The moment I heard that, a fear gripped me. I did not regret that I had helped the couple when they were undergoing emotional trauma. But my fear was what would happen to me. I went to the authorities and reported that this positive patient had been screened during my duty hours. I was advised to watch out for symptoms over the next seven days. After that they would do a test and that was that. Nothing happened for seven days and I was relieved. However, on the eighth day I developed slight fever and I was on the verge of panic. Why fever? Why now? I tried to look for reasons. Every morning I would take my bath before leaving home for duty. Once I finished my Covid duty, I was sprayed head to toe with D-125, a disinfectant. That would really drench me, clothes and shoes and all. Then I would reach home and take another warm bath. All that drenching must have caused the fever, I tried to justify. But there was still a 0.001 probability of infection and that was frightening. In isolation and on the edgeI went to the doctor on duty and told him I needed to get tested. He rolled his eyes and asked me why I had not told him before. But the seven days had gone off well, without any problem. How could I have told him before? “You may develop symptoms after 7 days or 14 days or even after 28 days. This virus is so tricky, the symptoms can come at any time. You must not take any chances,” the doctor explained. He called for the Medical Officer, who was in charge. My samples were taken. The Medical Officer spoke to me for about 45 minutes asking me the same questions over and over again, maybe just to check if I was consistent. By then, I was really very scared. Then he pronounced the verdict. He immediately sent me to the isolation ward for 24 hours. If the tests turned out negative, I would be quarantined for 14 days. “If the results come back positive, you know where we would send you,” he said ominously. All positive patients were being sent to a Covid facility in a different area, that had facilities for isolation and treatment. My throat was dry, my mind empty, and I had no idea what to do. After some time, I called up my husband and briefed him. Fortunately, I had sent my husband, my son and everyone else in my house to my father’s place, that was close to my house. When I did that, I was simply being very cautious as we were in a vulnerable location and I was dealing with Covid patients. I landed in the isolation ward. Yes, it was secluded. It was on the third floor of what we called the Covid building. It was scary to be all alone. The whole ward was silent. There was no conversation. Those who were on duty looked like robots, dressed up as they were in their protective suits. They never talked. They would come and do their job and then they would thoroughly wash their hands and go away. The silence was absolutely fearful. Emotionally breathlessI had simply not anticipated what lay ahead. There were so many messages and calls on my mobile, but I did not feel like responding. I had become very emotional and wanted to stay aloof from the world. I even switched off my phone; something I never do. Many fearful scenarios passed through my mind. I will never see my husband and son again. I will be moved to another isolation ward. If my immune system is not strong enough, the symptoms will start. Breathlessness would be the first. It is very difficult to even see someone else experiencing breathlessness. Because there is nothing you can do to help. It is so frustrating. I imagine myself struggling for breath with a ventilator pipe inside me. With all my knowledge and experience, I can’t bear to think of anybody trying to give me false hopes, telling me everything is okay, and I will be fine soon. I can’t see expressions of the medical staff around me. They are all wearing masks. Are they smiling at me? Are they frustrated? Are they angry? I can't see them. But they can see me. And that is so difficult to accept as a patient. Then sanity kicked in. Why am I shutting myself away? I am a professional, a healthcare worker, and this was to be expected. My friends are genuinely worried. Why am I pushing them away? I started replying to messages and returning calls. Positive thoughts follow a negative resultAfter almost 36 hours in isolation, my test results came back negative. And I am writing you this from home, where I have begun a 14-day quarantine. I am now so relieved. I am so grateful to all for their love. I just want to share my thoughts that would hopefully help someone somewhere somehow as we all go through this difficult phase. Those 36 hours spooked me, and I am supposed to be a doctor. Imagine people having to live through this for days together! It is so easy for us to point fingers at someone who is infected. But why not focus on what we can do to help? Can we spare some time and compassion to counsel a patient who has been sentenced to isolation? If someone in isolation is not eating (I did not) and not accepting calls, can we reach out and ensure that he or she has not slipped into depression? We may have to maintain distance physically. But should that stop us from getting close emotionally? This is when, more than medicine, you need comfort and care from a fellow human being. Now I am clear that I do not want sympathy. Neither did I do anything extraordinary. You may attribute it to my palliative care training, but I think a Covid-19 patient (proven or potential) deserves the same compassion and care that you would not hesitate to offer someone who is terminally ill. Today, I feel more charged up to carry on with what I am best at—providing palliative care. I have more than one reason to justify why it must be an important part of a humanitarian crisis. I wish to improve my skills, especially in the area of communication so that I can convince authorities to adopt a palliative care approach in every setting. And of course, the biggest challenge will be to demonstrate a visible change in the patient as well as the whole scenario of caregiving. I do hope that the science of palliative medicine will be allowed to play the key role it can, when we are trying to copy with such a calamity. We have the ability; we can reinforce the confidence. Will I go back to the screening area? Absolutely! I will go there and continue talking to people. I have seen the positive effect of a simple conversation. Yes, I cannot interfere in the isolation area. However, I have realized that there may be unknown fears in the minds of those working in the isolation ward. Perhaps, that explained their behaviour? I would like to tell those workers that they can talk to me, tell me about their fears. I am sure that would bring about a positive change in their approach, and ultimately benefit the patients. Personally, in the last few days, I have learnt the skill of detachment from worldly pleasures. They don’t mean anything unless you put a price tag to each. We do not know what tomorrow holds for any of us. At least today, when we still can, let us care for one another. That can be priceless. Based on a video posted by Dr Sanghamitra Bora and subsequent conversations with her.
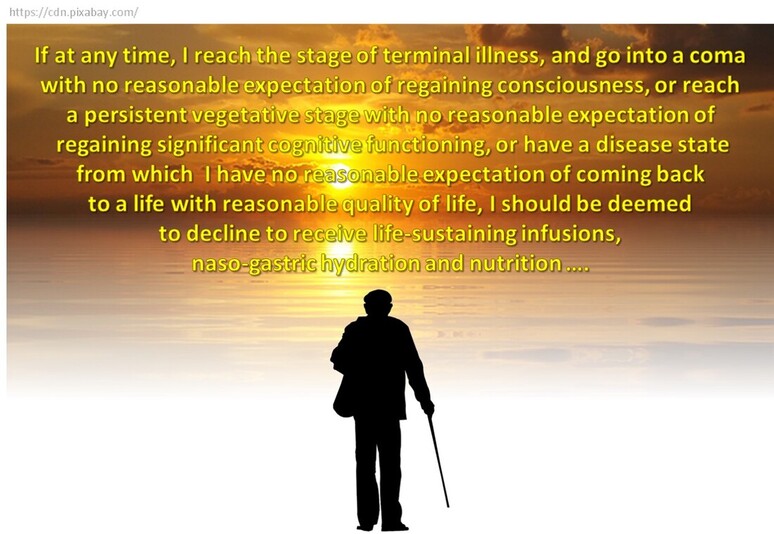
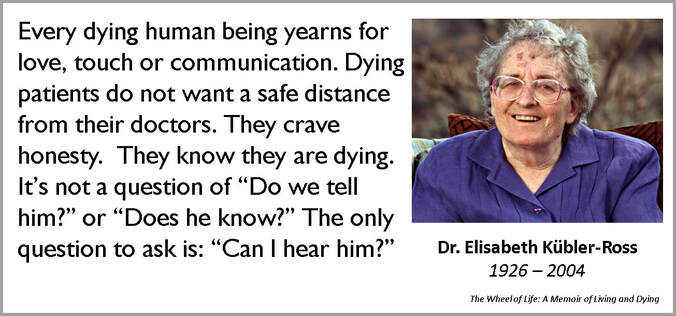
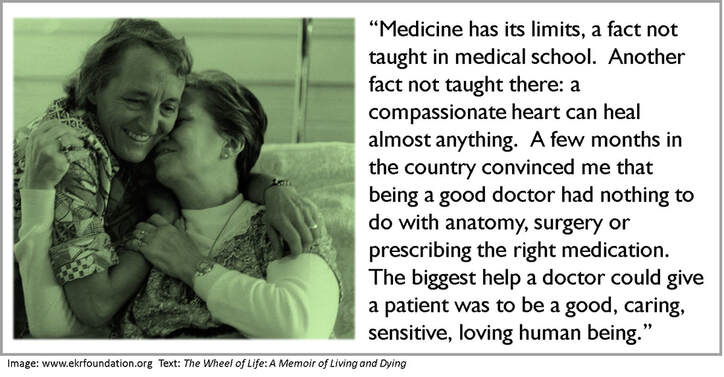
You know it is time. The disease has already won. You are ready to let go. But your family is not, nor are the doctors. As you lie there helpless, connected to so many tubes and machines, you sense your loved ones beyond the door, their fear, their sorrow. You wonder how they must be sacrificing to pay for all this. You want them to sit near you and hold your hand. And talk to you even if you can't respond. You want to tell them you love them and will always do. You know they love you, too. That is why you want them to remove all the tubes and machines. And just be with you at home, while you take leave. In peace, with dignity. If only you had told them how you wanted to go, when you could. The Guardian recently reported a study that found “the brain shields us from existential fear by categorising death as an unfortunate event that only befalls other people”. In other words, we are wired to deny life's only certainty, death. That being the case, it can be difficult to document our preferences about death. How can we think and discuss about how we want to be treated (or not) should we reach a terminal stage, a point of no return? But, think we ought to. Discuss we should. Document we must. The Supreme Court of India gave legal sanction to this “advance medical directive” or “living will” on March 9, 2018. The Supreme Court ruled that “in specific circumstances, a person has the right to decide against artificial life support by creating a living will,” and that “the right to life and liberty, enshrined under Article 21 of the Indian Constitution, also includes the right to die peacefully and with dignity.” Delivering the judgment, Chief Justice Dipak Mishra observed: “Should we not allow them to cross the door and meet death with dignity? For some, even their death could be a moment of celebration.” Will, living and deadDespite the ruling by the apex court, a living will remains a touchy issue. In 2015, three national medical associations of neurologists, intensivists and palliative care physicians came together to form the End of Life Care in India Task force (ELICIT). Dr Roop Gursahani, a consulting neurologist, who is part of ELICIT, says we “need to make conversations about death natural and not forced”. He points out that a living will “takes care of one’s healthcare decisions at the end of life." While living will formats can be easily downloaded from several sources (here is one), the government is yet to translate the Supreme Court ruling into enforceable procedures. Some experts feel what the court has suggested is too restrictive. You need to be certified terminally ill first, which may be too late. Also, the will needs to be countersigned by a judicial magistrate first class, who is not within easy reach of most people. Nevertheless, it is prudent to make a living will and communicate your preferences to your loved ones and those responsible for your health care. As it is difficult to plan for every eventuality, you can leave it to the discretion of one or two people whom you trust to implement your will. Financial planning Mention “will”, and one tends to think of a very legal-looking document. And of lawyers, and members of the family throwing not-necessarily friendly looks at one another. You also think of someone very ill, unlikely to be helped by all that he (or she) owns and has willed it away for others to enjoy. What matters most at the end is peace and dignity, at least for the patient. However, there is no wishing away the money elephant in the room. Fortunately, compared to the ethical and medical issues, planning for financial security is easier, provided you are willing to start long before it is time to make that final transition. Matters of money and anticipation when life is in transition A Certified Financial Planner, Sneha Jaggar recently qualified as a Financial Transitionist. Here she answers questions about finance and other issues at the time of life’s final transition. Q: Whether you wish to try everything possible to prolong life or decline heroic medical interventions, there are financial implications either way. How does one tackle this? Sneha: Life is a very delicate topic. My life is more precious to my near and dear ones than I perceive it to be. And this is often observed when a family member has to decide about treatment at the end of a loved one's life. These decisions are emotionally and financially draining if we do not know what the patient wants. You can help your family by having three things in place:
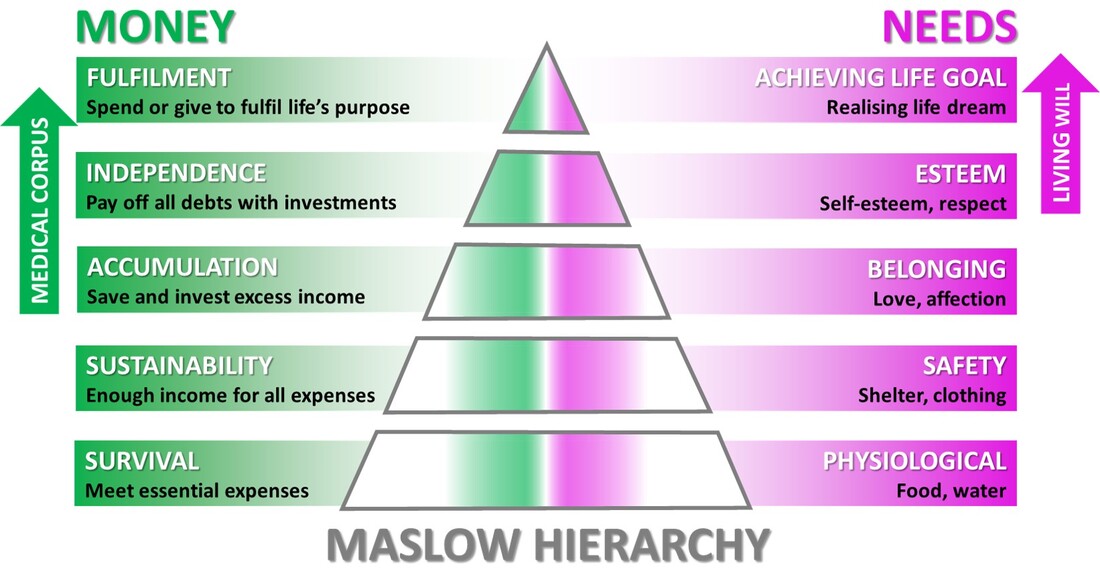
You help clients plan their life goals after retirement. Do you talk of terminal illness? Is it possible to quantify this requirement? Like I said, from the financial planning point of view, everyone should have the four basic insurance policies in place. However, as it keeps on increasing with one’s age, paying health insurance premium would be difficult after retirement. Additionally, medical inflation (cost of medical care) is presently the highest at 12% per annum. This is the reason why we need a separate medical corpus for the post-retirement period. When I speak to clients on retirement, I start by understanding their expectations. Many are practical. Some I need to sensitize about age-related illnesses. How much would they value their financial freedom should such a situation arise? The value of the corpus would depend on the individual and family, their standard of living, cash flow, net worth in the pre-retirement period, etc. These days parents prefer not to burden their children with end-of-life care. Do you have that conversation with the parent(s) or the children or both? Today, most parents are self-sufficient. However, they do need help in case of a medical emergency. Those who are still earning and want to be self-sufficient can build up a buffer for these emergencies. When I begin my conversations with parents, I try to understand where they stand in the Maslow hierarchy. When I know it is the right time to speak about legacy and wealth migration, I chart out detailed sessions with the parents first and then their children. During these sessions I speak not only about estate planning, but also about palliative care, end-of-life treatment and living will. Once the parents understand all this and are confident enough to talk about it, I involve the children. However, in spite of the Supreme Court ruling, the legal status and practical applicability of the living will remain hazy. Therefore, I tell my clients they should consult their doctors and lawyers about this. One son abroad is fully bearing the cost of treatment. The second son in India is the 24-hour caregiver but has no money. They have conflicting views on what is best for the patient, their father. How do you tackle such a situation? In this scenario of transition, both the sons are in what we call the anticipation stage. You expect an event (end of father’s life) to occur but that has not yet happened. Both the sons portray struggle traits in their behaviour. The one abroad is probably feeling helpless as he cannot be present physically. The other one is experiencing emotional fatigue, where he cannot see his father suffering in front of his own eyes. As a financial transitionist, I would use certain tools to help them clear their fears and frustrations. Then help them arrive at a decision that both are happy with and is best for the father, too. If one has drawn up clear plans after discussions, how to ensure those are enforced when the patient is totally helpless? For example, the patient may expect a certain course of action but the spouse may act entirely differently. I cannot speak on the legal position, but some of the issues here are that of understanding and expectation. Generally, financial planners/advisors talk about goals because they’re trained to craft them, and create timelines and benchmarks. Expectations are the spaces that exist in the narrative about goals. Some are vague, some are small, and some are fleeting. Regardless, they’re all important because they influence the thoughts and behaviour of the client. What makes expectations complicated is that they’re frequently not verbalized. Someone may or may not be correct about their perception of the expectations of others, even their near and dear ones. Regardless, expectations can create an unseen but powerful undercurrent that influences relationships, behaviour and satisfaction. When left unexplained while making important decisions, those details become little spaces of uncertainty that could create financial and personal problems. I help clients write down their assumptions and expectations regarding an event yet to occur. I also discuss the time horizons to gain greater clarity about why they have these expectations. Based on similarities and differences, I help determine the next steps most relevant to them. It could involve separate one-on-one discussions or joint sessions. This helps verbalize the thoughts and expectations one has of the other and brings the differences to light. Then it becomes easier to work towards a common ground. When is the right time to talk of the living will? Again, when I introduce this topic would depend on my comfort level with the client, his or her age, life circumstances, background and standard of living. For example, if I’m talking to a just-married couple, I will have to be rather sensitive about broaching the subject of a medical corpus. However, if either or both of them have already had close encounters of the medical kind involving someone close, they would be already sensitized. It would be easier to talk about medical corpus, end-of-life treatment and living will. In your opinion, what can be done to minimize confusion and ensure dignity at the end of life? Just to sum up, five actions can help a lot:
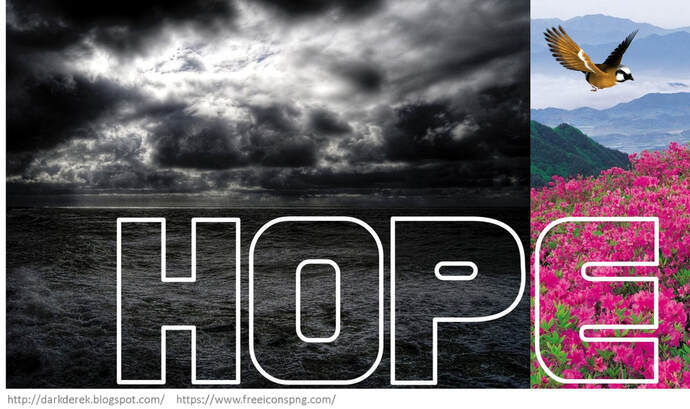
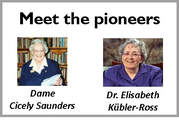
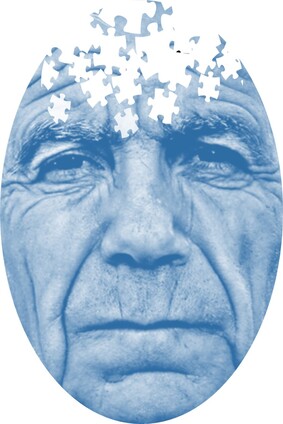
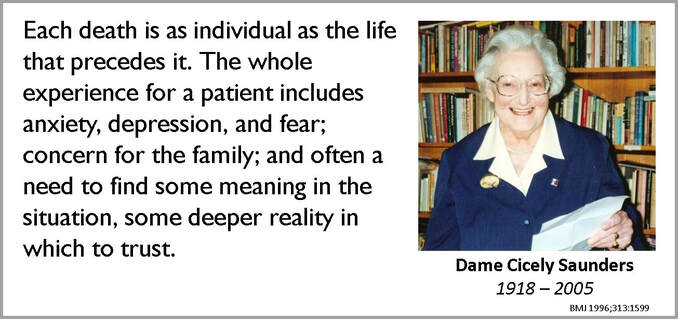
Have another question? Ask Sneha Jaggar. It was February. I stood barefoot on the beach, watching the waves rise and fall mightily, roll over my feet gently and then immediately return to meet the vast ocean. The evening sun spread its colours across the sky. Tiny boats dotted the horizon, returning to the shore. The smell of the sea filled my nostrils. I wondered how this came to be my life. How did I end up giving birth, then losing my 4-year-old daughter to cancer (brain tumour) after 18 months of struggle (of which 14 months were in palliative care)? How did my family and I survive the trauma? How did I come to stand on this beach without Ira? Clinging to elusive hopeI had noticed minor tremors in Ira’s left hand in March 2017. Initially it was attributed to motor development issues. After a few visits to the paediatrician and the neurologist, and a scan later, the diagnosis was confirmed—thalamic glioma. A surgery was imperative as the tumour pressed on several parts of the brain. All through, from diagnosis to surgery to post-surgery, hope remained a constant but its face kept changing. From hoping that the tremors would be non-worrisome, to thinking that the surgery would have no complications and to assuming that we’d be back home in 15 days. Ira’s treatment in the hospital lasted for 2.5 months. A major brain surgery and several post-operative complications later, Ira was in a state of poor consciousness. She had lost her speech and her ability to register and respond to stimuli around. In medical terminology, she was in a vegetative state. With each passing day, hopes of her recovery diminished. Our hopes for cure and recovery changed to hopes for comfort and relief for Ira. Help to hope rightAs a mother who went through it, I think there is confusion about hope during palliative care. It is not about giving and keeping false hopes about recovery or cure. Although, in our case, the acceptance of Ira’s condition took time to settle in, we learnt to keep any false hopes about her recovery at bay. We need to understand and accept the prognosis and course of treatment. There is no need to dismiss or discard hope. It just needs to be realistic. Focus on short-term goals and expect practical outcomes. Right through her palliative care, with all our love and compassion, we worked to provide as much comfort at home and as much relief from her neurological problems as possible. If a terminal patient or family member makes long-term plans or envisions a future with all, it is important for the medical and allied professionals to gently help them understand the prognosis. And tell them what hopes that they can realistically harbour. Hope beyond cureHope in palliative care, as complex as it may appear, is about several aspects except a cure. It should be about a good quality of life in the time left, reconciliation and closure with family members and friends, avoiding discomfort during the care, and being cared for with utmost love and selflessness. Though the tragedy of loss and the grief of death always stared us in the face, our family was content that distressing symptoms were reduced and managed at the earliest. As her mother and caregiver, I felt that Ira’s troubles, malaise and anguish were far greater than mine, and this gave me the strength to keep going and to care for her with even more compassion and love. Yes, hope is intangible. It will not just bounce into your life and light it up like fireflies at night. Find it within. Hang on to its threads as if your life depends on it, because it really does. Pratima Mehta writes a blog about Ira’s journey, how the family coped and practical aspects of care. ALREADY PUBLISHED IN THIS SERIES This story is about Madhav and Eknath (both about 75). Two different men and their families, who do not have much in common. Except for a common villain, dementia. This story is about how palliative care is helping them cope. I started looking after Madhav following a phone call. “Can you help my mom? My father is a dementia patient. My sister and I live out of India. My mother has difficulty managing him. Can you make home visits?” With Eknath too, the starting point was a call. However, the caller was clueless about the diagnosis. “Can you help my uncle?” Sure! What sort of help? “I don’t know. I need your guidance.” "Why can't he behave?"Both Madhav and his wife have chronic medical conditions. He has dementia and heart issues. She has kidney problems, diabetes and blood pressure. Their daughters who live abroad try to manage things remotely. There is no other family support. The first thing the wife told me was, “He does not remember anything, does not want to do anything and doesn’t co-operate. I don’t understand why he is doing all this to me. Why can’t he just behave properly? He was okay until a few months back.” “You do know that he has dementia, right?” I tried to make that question sound as gentle as possible. “Yes, I know that. That is okay. What about the other things he keeps doing that trouble me?” Would prefer to, but can't be aloneEknath is unmarried. He was a professor in a small town, lived alone, self-sufficient. He has always been on good terms with his siblings and their children. No longer working, he was keen to spend the rest of his life in that small town that had been his home for so long. But fate had other plans for him. Worried by his repeated falls at home, his neighbours requested his nieces and nephews to take him to a place closer to them. Thus, after 40 years, he ended up in the big city of Pune. Investigations suggested the beginning of Parkinson’s. One of his nieces volunteered to accommodate him in her house. But he was not comfortable there. He did not want to be an extra burden as his brother was already a Parkinson’s patient and needed constant attention. Eknath became aloof and would not co-operate. They decided to let him to stay separately, with someone visiting him frequently. This arrangement lasted for a few months. However, as his symptoms worsened, it became difficult. When I visited him, his cognitive abilities were intact, he could recognise people and he was alert. Helping the spouse copeIn another part of Pune, as I started working with Madhav, I realised that many of his cognitive abilities were affected. He could not comprehend what he was reading, nor could he complete any activity on his own. But I decided to make the wife my first priority. We had a few issues in the beginning, but I managed to develop a good rapport with her by and by. I had to make her understand the whole spectrum of dementia and how to cope with his behaviour. In the course of our conversations, I discovered that apart from watching TV and playing solitaire on the laptop, she could draw well and liked to solve word puzzles. She did have some drawing material lying around but those were in a bad shape. She was not very keen to spend on her hobby, but I persuaded her to get some new stuff and arranged for some puzzles. Soon, she got going and was happy in her own space. "This is an invasion of privacy"In the case of Eknath, it took some coaxing before Eknath agreed to employ a caregiver for the day. “I don’t want anybody in the house, I can manage myself,” he was still the proud, independent professor. Eknath had not been to a doctor for more than two years. I suggested a visit to the neurologist. Tests confirmed early dementia. Marking a new phase in his life, Eknath started taking medicines and slowly got used to the caregiver. There were more falls and serious issues with hygiene and nutrition. The caregiver had to start staying nights, too. “This is an invasion on my privacy,” Eknath protested. We were all helpless. We pleaded with him to try it out for a few days. He agreed reluctantly. I helped set some rules and regulations for the caregiver, who had had no professional training. I also used my weekly visits to build a good rapport with Eknath. We would do a lot of activities together—games, puzzles, drawing, painting, craft work and so on. They all cared for him, but the nieces and nephews could not spare too much time from their respective lives. Except for his siblings and some old students, he had no social visitors. Life appeared to be under control. Boosting the support systemMeanwhile, Madhav was having his good days and bad days. Did they have any doctor on call to help them out, in case …. No! Any relative? “Well, I have a cousin. She is old. But she can come when needed.” That did not sound very promising. I was constantly in touch with Madhav’s daughters. They arranged for a local doctor to come home and guide them. We also managed to locate a younger member of the extended family, who was willing to come whenever Mrs Madhav needed any help. I gave them a few tips on making optimum use of the support system now in place. When to call for the doctor, when to hospitalise, how to manage the caregiver and so on. I helped them prepare their home for the long-time care of a dementia patient—caregivers, Fowler bed, essential medicines. I also got them to involve a step-down centre where he could be admitted for symptom management. They also engaged a palliative care physician. I involved the family in long discussions with the experts—what to expect, likely difficulties and how to manage those. “How do you want your father to be cared for?” I asked both the daughters. “Do everything possible,” one said. “I want him comfortable,” said the other. Two different perspectives. As it happens very often, I knew this conversation would be long and slow. “Where do you want your father to be? At home or in a hospital?” “Home, of course.” Mother can manage him best at home. Initially, the daughters were unsure about involving the mother in the discussions. What would she know? Well, she surprised everyone. During the discussion with the palliative care specialist, Mrs Madhav clearly demonstrated she was now assessing the situation objectively and was ready to cope with comfort care. Both the daughters also concurred that comfort and quality of life were important. All these discussions got the daughters worried. “Is father so ill? Should we come down to see him? We want to be there when he is really bad and when mother needs us most,” they told me. “I understand that,” I told them. “But how about coming now? When your father can still recognise you? You can spend quality time your parents. You will always cherish those memories, whatever the future holds.” A turn for the worseOne day, Eknath had a nasty fall. That necessitated a surgery followed by another. Old difficulties like incontinence, hygiene problems and behavioural issues started worsening. A local doctor was arranged to take care of his physical symptoms . Meanwhile, the need to provide constant care day and night took a toll on the caregiver. He suffered a burnout and the quality of care dropped. It was time to look for a more lasting solution. That triggered a debate among the members of the family. “Why not keep him in an assisted-living centre? He will be well cared for.” “But for how long?” “Maybe he should move back to his hometown? That’s what he wants.” The discussions went on until they decided to keep him in a centre under medical supervision. Peacefully ever afterThe journey continues. Madhav’s daughters have already come home more than once and have spent time with father. As he continues to move away from them in body and spirit, they are more in control of what is happening. Mother and daughters are more at peace. At the centre, Eknath’s health has improved slightly. They have started him on physiotherapy. There are people around he can interact with. At the request of the family, I have been regularly visiting him at the centre. He repeats one question, “When do I go home?” Are you not comfortable here? “Yes, I am. But I want to go home.” Eknath’s family and well-wishers are still discussing. There are some tough decisions to take. Everyone means well. Everyone wants a say. Except for their names, Madhav and Eknath are for real. They face difficult questions and the answers are not easy to come by. As dementia worsens, palliative care will help them remain free from pain and distress. Until .... Until and after, science and compassion will continue to help them all cope and find peace. Madhura Bhatwadekar, Palliative Care Social Worker ALREADY PUBLISHED IN THIS SERIES When I met her the first time, she was on a wheelchair, in severe pain and was being treated for pancreatic cancer for nearly three years. Her husband, her primary caregiver, was with her. I studied her papers and examined her. I asked her if her ascites (fluid in the abdomen) was causing her discomfort. She was willing to manage. The next contact was about 12 days later, when the husband called. She had been recommended an MRI. He asked me if it made sense to push her through yet another MRI. Then he came over to talk to me . Their two sons were abroad. Financially, they were comfortable. They lived on the fourth floor and the building had no lift. Every hospital visit meant maneuvering her down the stairs. He was willing to do that. But to do that every time? Won’t it be difficult for him to manage her at home? Dealing with at-home careI briefed him about the potential challenges of at-home care. Perhaps it was time for him to have a frank conversation with her doctor about the prognosis? One week later I got a request to visit the patient at home. The doctor had said that her treatment was now at a palliative phase. Thanks to that, the husband had a better idea of my role as a palliative care doctor. I examined the patient. It was obvious that her disease was progressing rapidly. She looked jaundiced. No, she still did not want her ascites to be drained. She looked at peace, pretty even. She had just one fear. Occasionally, when she got up, she felt as if she was about to fall. Now that I was with her, I encouraged her to try and get up. With my help, she did. She was stumbling. It was clear to me that she was wobbly. After safely putting her back in bed, I suggested several measures. She was not to be allowed to get up and walk without support. Never. And she needed a hospital bed with rail guards. His brother walked with me as I took the stairs down. He was not sure if the sons had the correct picture. I suggested he could share my number with one of them and I would be happy to brief them. He was relieved. That evening, before I could speak to the son, I got a call from the brother. The patient had had a fall. They had rushed her to the ICU in a nearby hospital. Spend time together nowWhile the immediate injury was being taken care of at the hospital, I got a call from the son in the US. I briefed him fully and answered his questions. He said he was coming to India towards the end of the month, three weeks away. If he wanted to spend some quality time with his mother, I suggested he should reach sooner. The next call I received was again from the same son but after he had reached the hospital in Pune. He had met his mother and she had recognized him, smiled at him. He was happy. A couple of days later, the husband’s brother called again. She was not doing well at all. The second son too was on his way. He too got to meet mother, but she was already on ventilator. The family had a discussion with the doctor. How long should she remain on the ventilator? The sons decided to wait until the next evening. But she did not wait. She passed away the next morning, in the ICU. If only ...A few days later, the son spoke to me. “We knew her disease was serious. She was so keen to be at home. Dad was trying to make it possible. I desperately wanted her to get comfort care, like what we get in the US. Then after all those months of suffering, she got to meet you. Thank you for asking me to come down sooner than I was planning to. I got to meet her, spend some time with her.” He was sobbing bitterly. I told him that all I did was try to make the journey smooth. For the traveler and her dear ones who were around to see her off. She was gone. But those moments together, those memories would stay. When it comes to a terminal condition, is it possible to prognosticate the end with any certainty? Would the ending have been less painful for all, had there been franker conversations sooner? Could they have then made better use of the time with her? Dr Priyadarshini Kulkarni, Palliative Medicine Consultant, Pune. Founder, EaseandSupport ALREADY PUBLISHED IN THIS SERIES These days we have several days dedicated to one thing or the other. Tomorrow, October 12, 2019, is earmarked for something that concerns life and death, the comfortable, dignified transition from one to the other and life thereafter. The second Saturday of every October is World Hospice and Palliative Care Day. Unless you catch a stray headline or a post brushes by while you wade through social media, you may miss the significance of October 12, 2019. Unless you suffer from a chronic illness or you care for someone who does, or you help both as a palliative care professional. In which case, it is a day that would probably mean the world to you. This is the right occasion to remember two women who were strong enough to be compassionate. They were both discouraged from the medical profession when they started their education. Then the world plunged into war and they boldly went into the uncommon profession of compassionate care. They deliberately chose to sit next to and hold the hand of pain and misery. So that they could teach an uncaring world to understand and manage both, and death, better. Meet Dame Cicely Saunders and Dr Elisabeth Kübler-Ross, the Pioneers of Compassionate Care. Dame Cicely Saunders |
AuthorVijayakumar Kotteri Categories
All
Archives
April 2024
|





































 RSS Feed
RSS Feed